For decades, NHS pathology departments have relied on locum pathologists to plug service gaps. At first, the model worked. The pool of highly qualified locums was large enough to cover shortfalls, and departments could lean on temporary contracts as a quick fix.
But today, that safety net has worn thin. The number of available locums has plummeted, while demand for pathology services has soared, particularly in subspecialist areas such as paediatric, ophthalmic, and perinatal pathology.
The scale of the problem is stark:
Behind these statistics are patients waiting longer for vital answers, sometimes weeks for a cancer diagnosis and clinical teams forced into unsustainable overtime just to keep services moving. What was once a stop-gap is now a critical vulnerability. Locum contracts are harder to fill, more expensive, and less efficient. NHS departments need more than short-term fixes: they need a sustainable way to secure diagnostic resilience.
The timing has never been better. Over the last five years, NHS pathology has undergone a quiet but significant shift.
Concerns about digital equivalence have also been resolved. Large-scale validation studies confirm that whole-slide imaging (WSI) matches the diagnostic quality of glass slides and in many cases, offers faster turnaround and better subspecialist access.
Every day saved in reporting time can mean faster treatment decisions, earlier interventions, and less anxiety for patients. Digital pathology isn’t just about efficiency, it’s about giving clinicians the timely information they need to save lives.
The foundation for a more resilient, modern service model is already in place. The question is how to scale it.
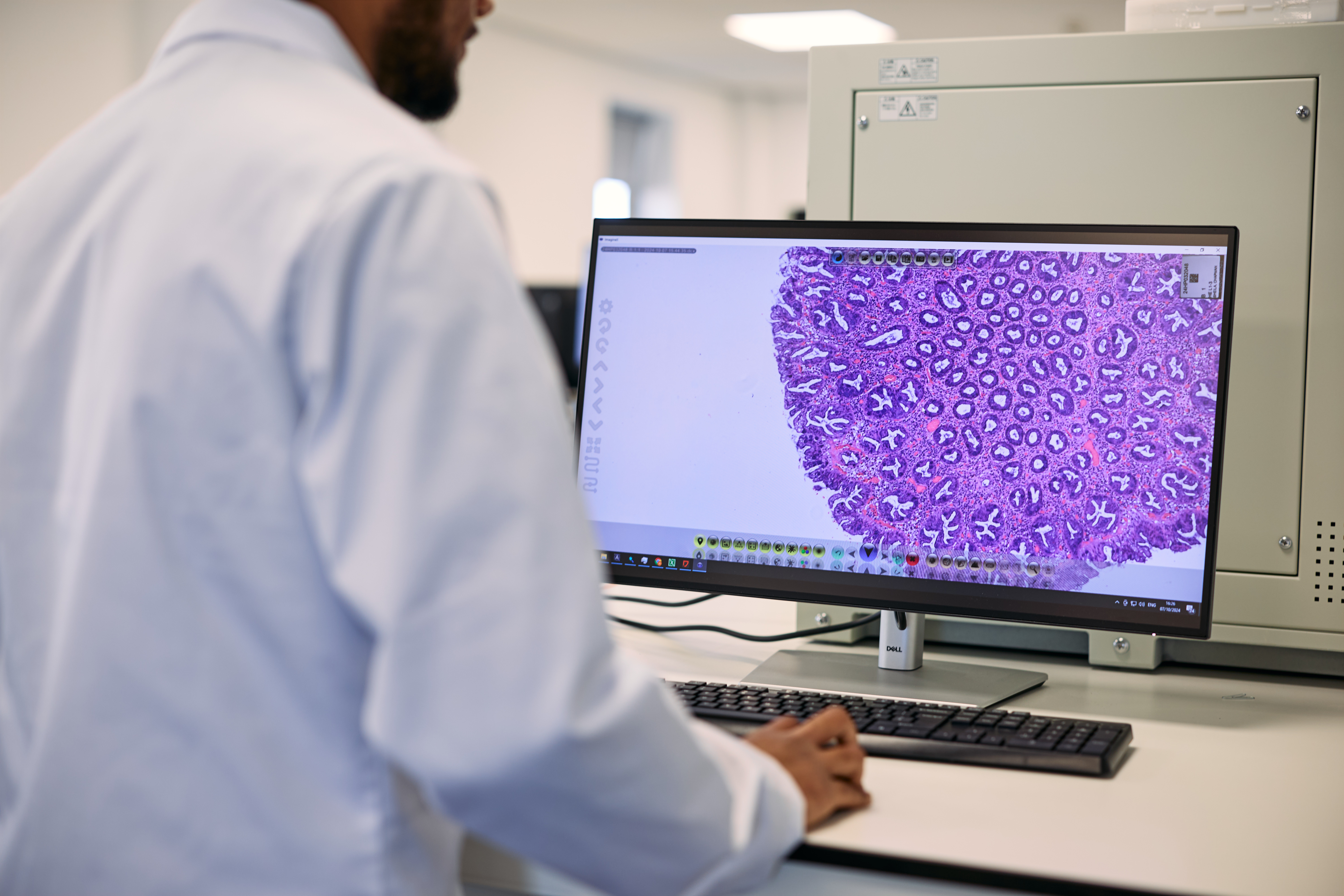
At Diagnexia, we’ve built a network of GMC-registered, subspecialist pathologists working on our proprietary, AI-enhanced digital pathology platform. Unlike the locum model, we don’t require onboarding delays, physical desk space, or IT setup. Instead, we integrate directly into your existing workflow, whether through local scanners and LIS systems, or via digitisation at our scanning centres in Oxford and Exeter.
The result is a seamless, virtual extension of your diagnostic team, offering:
A complex sarcoma or paediatric case shouldn’t wait for the right expertise to be found. With Diagnexia, subspecialist knowledge is always within reach, ensuring patients receive accurate diagnoses and care plans without delay. This isn’t a temporary patch. It’s a long-term, integrated service that makes diagnostic resilience achievable.
One frequent objection to remote pathology is the issue of specimen dissection (cut-up). Historically, this required onsite pathologist presence. But the reality is evolving:
Far from being a limitation, this evolution frees pathologists to focus more time on what matters most: expert diagnosis and patient care. Diagnexia supports local strategies to ensure this step of the workflow is fully covered.
Let’s be clear: reliance on locum contracts introduces systemic risks that NHS departments can no longer ignore. Locums create:
Meanwhile, departments still face rising costs, scarce availability, and increasing turnaround pressure. It’s not just inefficient, it’s unsustainable.
By contrast, Diagnexia provides always-on, specialist capacity at a fixed, predictable cost, without the administrative complexity.
Pathology is not just a laboratory function, it is the foundation of cancer and elective care. When diagnostic reporting stalls, entire patient pathways stall. Locum contracts may once have bridged the gap, but today they put both patient timelines and clinician wellbeing at risk.
With Diagnexia, NHS departments gain:
This is about more than contingency planning. It’s about embedding resilience at the heart of diagnostics, so departments can keep pace with national targets, safeguard patient outcomes, and future-proof against workforce shortages.
Every week lost to contract negotiations, onboarding, or delays adds to the backlog of patients waiting for answers. Locum contracts cannot deliver the resilience the NHS needs.
With Diagnexia, you can secure expert reporting, subspecialist access, and digital resilience, without the inefficiencies of temporary staffing.
Speak to our team today and take the first step toward building a sustainable, resilient diagnostic service.
For decades, NHS pathology departments have relied on locum pathologists to plug service gaps. At first, the model worked. The pool of highly qualified locums was large enough to cover shortfalls, and departments could lean on temporary contracts as a quick fix.
But today, that safety net has worn thin. The number of available locums has plummeted, while demand for pathology services has soared, particularly in subspecialist areas such as paediatric, ophthalmic, and perinatal pathology.
The scale of the problem is stark:
Behind these statistics are patients waiting longer for vital answers, sometimes weeks for a cancer diagnosis and clinical teams forced into unsustainable overtime just to keep services moving. What was once a stop-gap is now a critical vulnerability. Locum contracts are harder to fill, more expensive, and less efficient. NHS departments need more than short-term fixes: they need a sustainable way to secure diagnostic resilience.
The timing has never been better. Over the last five years, NHS pathology has undergone a quiet but significant shift.
Concerns about digital equivalence have also been resolved. Large-scale validation studies confirm that whole-slide imaging (WSI) matches the diagnostic quality of glass slides and in many cases, offers faster turnaround and better subspecialist access.
Every day saved in reporting time can mean faster treatment decisions, earlier interventions, and less anxiety for patients. Digital pathology isn’t just about efficiency, it’s about giving clinicians the timely information they need to save lives.
The foundation for a more resilient, modern service model is already in place. The question is how to scale it.
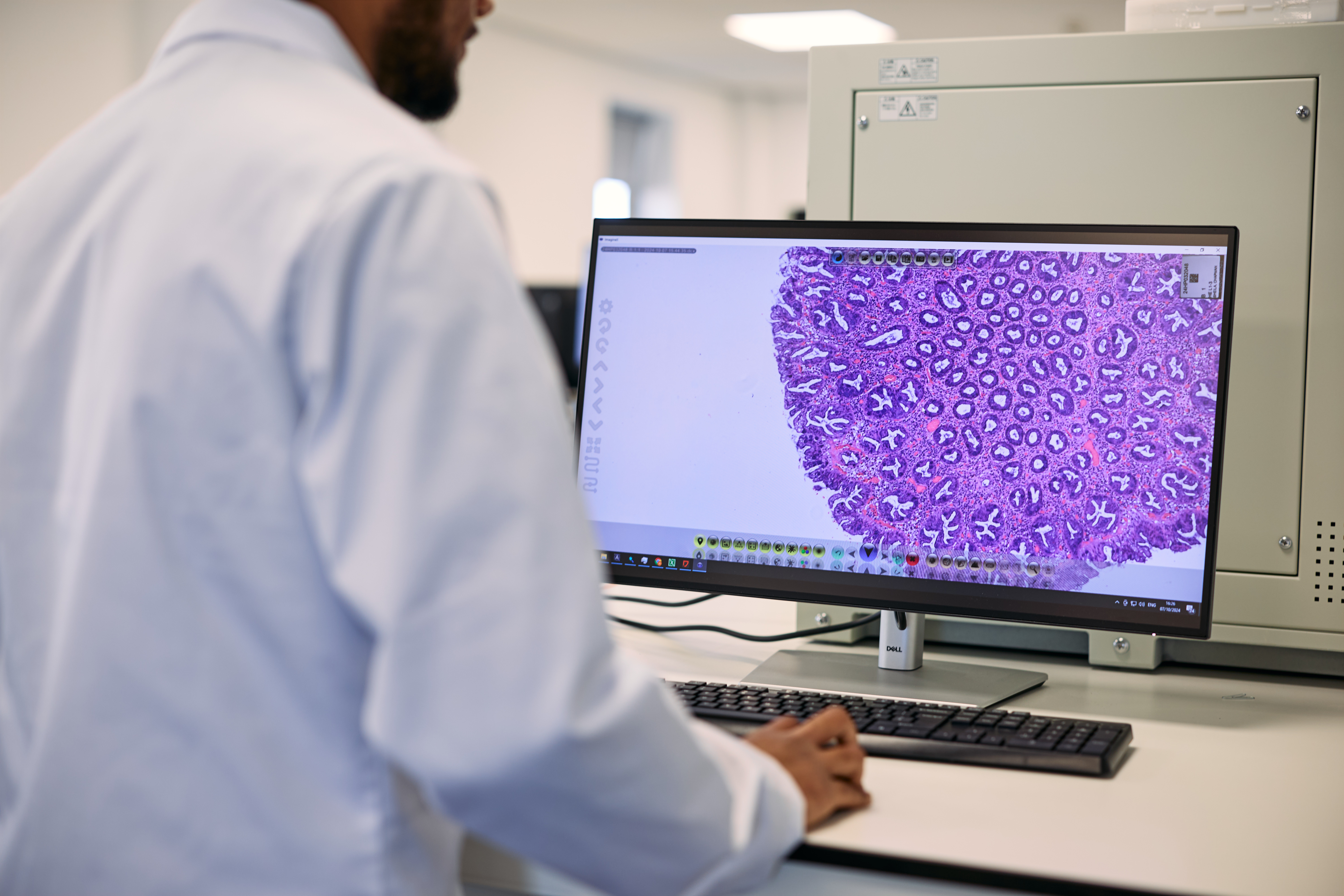
At Diagnexia, we’ve built a network of GMC-registered, subspecialist pathologists working on our proprietary, AI-enhanced digital pathology platform. Unlike the locum model, we don’t require onboarding delays, physical desk space, or IT setup. Instead, we integrate directly into your existing workflow, whether through local scanners and LIS systems, or via digitisation at our scanning centres in Oxford and Exeter.
The result is a seamless, virtual extension of your diagnostic team, offering:
A complex sarcoma or paediatric case shouldn’t wait for the right expertise to be found. With Diagnexia, subspecialist knowledge is always within reach, ensuring patients receive accurate diagnoses and care plans without delay. This isn’t a temporary patch. It’s a long-term, integrated service that makes diagnostic resilience achievable.
One frequent objection to remote pathology is the issue of specimen dissection (cut-up). Historically, this required onsite pathologist presence. But the reality is evolving:
Far from being a limitation, this evolution frees pathologists to focus more time on what matters most: expert diagnosis and patient care. Diagnexia supports local strategies to ensure this step of the workflow is fully covered.
Let’s be clear: reliance on locum contracts introduces systemic risks that NHS departments can no longer ignore. Locums create:
Meanwhile, departments still face rising costs, scarce availability, and increasing turnaround pressure. It’s not just inefficient, it’s unsustainable.
By contrast, Diagnexia provides always-on, specialist capacity at a fixed, predictable cost, without the administrative complexity.
Pathology is not just a laboratory function, it is the foundation of cancer and elective care. When diagnostic reporting stalls, entire patient pathways stall. Locum contracts may once have bridged the gap, but today they put both patient timelines and clinician wellbeing at risk.
With Diagnexia, NHS departments gain:
This is about more than contingency planning. It’s about embedding resilience at the heart of diagnostics, so departments can keep pace with national targets, safeguard patient outcomes, and future-proof against workforce shortages.
Every week lost to contract negotiations, onboarding, or delays adds to the backlog of patients waiting for answers. Locum contracts cannot deliver the resilience the NHS needs.
With Diagnexia, you can secure expert reporting, subspecialist access, and digital resilience, without the inefficiencies of temporary staffing.
Speak to our team today and take the first step toward building a sustainable, resilient diagnostic service.